Esophagitis is the inflammation or irritation of the esophagus, also known as esophageal mucosal damage. It is the most common complication of GERD. Causes of esophagitis include acid reflux from the stomach into the esophagus, infections, allergies, and certain medications. Esophagitis can progress to serious complications if left untreated.
Introduction
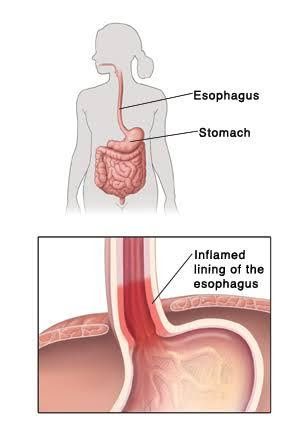
Esophagitis is the inflammation that may damage tissues of the esophagus. The esophagus (food pipe) is a muscular tube that connects your mouth and your stomach. When the esophagus gets inflamed, it makes swallowing difficult and painful and causes chest pain.
Esophagitis is caused by conditions such as acid reflux or gastroesophageal reflux disease, viral, bacterial, and fungal infections, allergens, and certain drugs. Management of esophagitis depends on the cause and the severity of the condition.

Untreated and long-term esophagitis can destroy the lining of your esophagus and affects its ability to deliver food from the mouth to your stomach. Complications of esophagitis include esophageal stricture, that is, scarring or narrowing of the esophagus, esophageal tears, and Barrett’s esophagus.
Causes of Esophagitis
Esophagitis can be caused by different conditions. In some cases, two or more factors may be the cause. Thus, esophagitis is categorized according to the underlying conditions causing it. These include:
Reflux Esophagitis
There is a muscular junction between the esophagus and the stomach called the lower esophageal sphincter (LES). It acts like a valve, opening to allow food to enter your stomach when you eat. Then, it closes to prevent the backflow of acidic contents into the esophagus.
If the LES opens when it shouldn’t or doesn’t close properly, the food and digestive acids may flow back into the esophagus (gastroesophageal or acid reflux). Gastroesophageal reflux disease (GERD) is a condition in which this acid reflux is persistent. A common complication of GERD is esophagitis- chronic inflammation and damage of the esophageal tissue.
Eosinophilic Esophagitis
Eosinophils are white blood cells key in mediating allergic reactions. Eosinophils can cause esophagitis when they are present in large numbers in the esophagus. This is often in response to a foreign agent such as an allergen or acid reflux or both. Allergens are agents that cause allergies.
In many cases, eosinophilic esophagitis may be triggered due to food allergies. Foods that people are most sensitive to include milk and other dairy products, eggs, wheat, soy, shellfish, peanuts, rye, beans, tree nuts, and beef.

Nonfood allergies can also cause eosinophilic esophagitis in some people. Environmental allergens such as pollen, dust mites, and molds may contribute to this condition in some cases.
Drug-induced Esophagitis
Improper use of several medications may cause tissue damage to the lining of the esophagus. Improper use refers to taking a pill with little or no water. This makes it possible for the pill or its residue to remain and have prolonged contact with your esophageal lining. Classes of drugs that may cause esophagitis include:
- Pain-relieving medications. Examples are ibuprofen, aspirin, and naproxen sodium.
- Antibiotics. Examples include tetracyclines, particularly doxycycline, clindamycin, amoxicillin, ciprofloxacin, and metronidazole.
- Potassium chloride. A drug used to treat potassium deficiency.
- Bisphosphonates. This class of drugs is used to prevent and treat bone loss. An example is alendronate (Fosomax), a drug used to treat osteoporosis.
- Quinidine. A medication used to treat cardiac problems.
Lymphocytic Esophagitis
Lymphocytes are a type of white blood cell. They play a role in fighting off infections. Although a rare condition, lymphocytic esophagitis (LE) occurs when lymphocytes are in high concentration in the lining of the esophagus. LE may be linked to GERD or eosinophilic esophagitis.
Infectious Esophagitis
Infections (caused by bacteria, viruses, or fungi) in the esophagus may result in esophagitis. Candida albicans, a fungus present in the mouth is a common cause of infectious esophagitis.
Infectious esophagitis is frequently seen in people who are immunocompromised (have weakened immune systems). These include people with disease conditions like HIV/AIDS, cancer, and diabetes, and on medications like steroids or antibiotics. However, this condition is rare.
Risk factors for Esophagitis
Risk factors for esophagitis depend on the cause of the esophagitis.
Reflux Esophagitis
These factors are similar to the factors that cause GERD. They include:
- Eating habits such as eating large meals, or late at night
- Eating fried meals, fatty meals, foods (and beverages) like alcohol, caffeine, chocolate, and mint-flavored foods

- Smoking and exposure to second-hand smoke
- Obesity or being overweight
- Pregnancy
Foods that can worsen reflux esophagitis include tomato-based foods, citrus fruits, caffeine, alcohol, spicy foods, garlic and onions, chocolate, mint-flavored foods.
Eosinophilic Esophagitis
Risk factors for eosinophilic (allergy-related) esophagitis include:
- A history of certain allergies or allergic reactions. Examples include bronchial asthma, allergic rhinitis, allergic dermatitis, etc.
- A family history of allergies or eosinophilic esophagitis
Drug-induced Esophagitis
Risk factors of drug-induced esophagitis refer to conditions or problems that prevent the smooth and complete passage of a pill into the stomach. They include:
- Taking a pill with little or no water
- Taking medications while lying on your back
- Taking drugs just before going to bed. This could be related to decreased production of saliva or reduced swallowing reflex during sleep.

- Older age, related to the age-related weakened muscular function of the esophagus or decreased production of saliva
- Swallowing large or oddly shaped pills
Infectious Esophagitis
Risk factors for infectious esophagitis are mostly related to medications (steroids and antibiotics) and disease conditions that weaken immunity. These include HIV/AIDS, cancers, diabetes, and immune disorders. People with diabetes are at a higher risk of candida esophagitis.
Treatments of certain cancers (chemotherapy and radiation therapy) may increase the risk of infectious esophagitis. Also, immunosuppressants (drugs that prevent or reduce immunological reactions) given to prevent organ transplant rejection or treat autoimmune diseases may predispose patients to infectious esophagitis.
Symptoms of Esophagitis
Common signs and symptoms of esophagitis include:
- Dysphagia- difficult swallowing
- Odynophagia- painful swallowing
- Sore throat/hoarse voice
- Chest pain (occurs or worsens with eating)
- Heartburn
- Nausea
- Vomiting
- Acid reflux
- Decreased appetite
- Food impaction- food gets stuck in the esophagus while swallowing
- Abdominal pain
- Cough
You may notice the following in infants and young children as they may be unable to voice out their pain or discomfort:
- Difficulty feeding
- Failure to thrive
Symptoms of esophagitis are similar to symptoms of other digestive disorders. Contact your doctor if symptoms:
- Persist for more than few days
- Are not relieved with over-the-counter antacids
- Are severe enough to cause feeding difficulties
- Are accompanied by symptoms like fever, headache, and muscle aches.
Seek emergency care if you:
- Experience chest pain that lasts more than a few minutes, especially if you have a history of high blood pressure, heart disease, or diabetes.
- Feel pain in your mouth and throat when you eat
- Have food stuck in your esophagus
- Vomit forcefully or in large amounts. Also, if the vomit looks yellow, green, brown (like coffee grounds), or is bloody.
- Experience shortness of breath shortly after eating or vomiting.
Medications for Esophagitis
Medications depend on the type of esophagitis.
Reflux Esophagitis
- OTC (over-the-counter) medications:
- Antacids, H2-receptor blockers, and proton-pump inhibitors (PPI). Examples of antacids include aluminum hydroxide (ALternaGEL, Amphojel) and magnesium hydroxide (Phillips Milk of Magnesia, Phillips Chewable). H2-receptor blockers are medications that reduce acid production like cimetidine (Tagamet), ranitidine, nizatidine, and famotidine (Pepcid). Proton-pump inhibitors (PPI) are medications that block acid production, thus healing the esophagus.
- Prescription-strength medications:
- Medications prescribed are often H2-receptor blockers and proton-pump inhibitors (PPI). Prokinetics may also be prescribed. They help your stomach empty faster so that you do not have much acid in it. Examples are metoclopramide (Reglan) and bethanechol.

Eosinophilic Esophagitis
Treatment for this condition is aimed at avoiding the allergen and reducing the allergic reaction with medications. Medications may include:
- Proton pump inhibitors (PPIs):
- This is usually the first type of medication your doctor will prescribe. Examples include lansoprazole (Prevacid), omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix).
- Steroids:
- These medications act topically and treat eosinophilic esophagitis. Examples of steroids include fluticasone (Flovent), and budesonide (Pulmicort). Some asthma medications may also be prescribed. Instead of inhaling these medications, they are swallowed and allowed to coat your esophagus. Their delivery system prevents adverse side effects than oral steroid pills.
Drug-induced Esophagitis
Instead of prescribing medications, treating drug-induced esophagitis focuses on alternative ways to take the drug and/or how you take the original drug. Your doctor may prescribe:
- An alternative drug that has a lower risk index for drug-induced esophagitis
- A liquid version of a medication if available
The following may also be recommended:
- Drinking enough water (e.g. a glass of water) with a pill. This may not be followed if your doctor asks to watch your fluid intake, usually because of a renal disease and heart disease
- Sitting or standing for at least 30 minutes after taking a pill.

Infectious Esophagitis
Your doctor will prescribe a medication(s) that will attack the causative organism of the infection.
- Antibiotics
- Antiviral medication
- Antifungal medication
Surgeries for Esophagitis
Surgeries may be indicated if other interventions do not work. It may also be used to treat complications of esophagitis such as food impaction. Surgical procedures include:
Reflux Esophagitis
- Fundoplication:
- This procedure involves wrapping the top of the stomach around the lower esophageal sphincter (LES). The procedure strengthens the sphincter, increases pressure at the lower esophagus, and prevents acid reflux. Fundoplication can be carried out through laparoscopy (crating small holes through the abdomen) or through open surgery
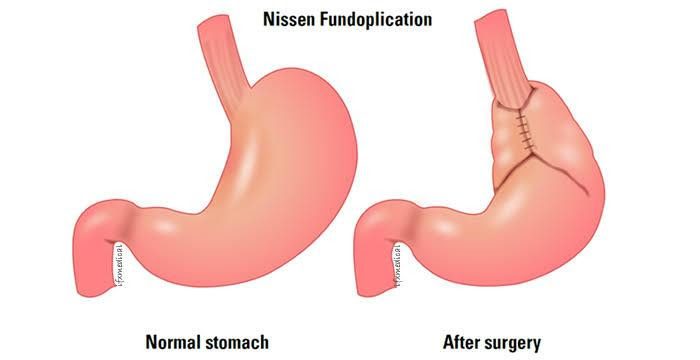
- Transoral incisionless fundoplication (TIF):
- This surgery involves the use of an endoscope (a small tube with a camera) to wrap the stomach around the LES with tweezers and plastic fasteners. It is less invasive, requires less treatment time, provides less pain and faster recovery than laparoscopy.
- Stretta procedure:
- This procedure uses low radiofrequency heat to produce burns to tighten the muscle of the LES. The doctor achieves this by passing a small tube down the esophagus.
- LINX surgery:
- The surgeon uses a device to reinforce the LES. The device is a flexible band of interlinked magnetic titanium beads placed around the LES. The magnetic attraction of the beads breaks temporarily to make food pass and enter the stomach. However, it is tight enough to prevent reflux.
Food impaction/Esophageal Stricture
- Esophageal Dilation:
- This procedure is performed when there is severe narrowing of the esophagus (esophageal stricture). It can also be done to relieve food impaction (when food is stuck in the esophagus). The gastroenterologist uses one or more endoscopic devices. These devices may be equipped with:
- A tapered tip with rounded point that slowly widens
- A balloon that can be inflated after it is passed into the esophagus.
Lifestyle Changes for Esophagitis
Lifestyle changes depend on the type of esophagitis. The following lifestyle modifications may help prevent recurring problems or relieve symptoms:
- Avoid Foods Triggers:
- This refers to foods that increase reflux, relax the LES or worsen symptoms of esophagitis. These foods include fatty and fried foods, spicy foods, mint-flavored foods, chocolate, caffeine, alcohol, pepper, citrus fruits and juices, onion, garlic, and tomato-based products.
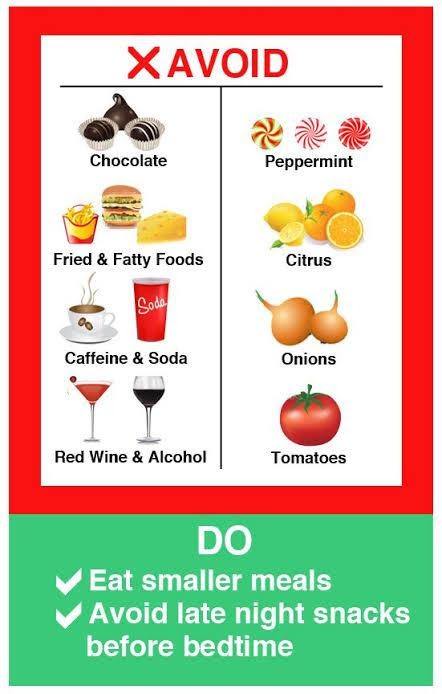
- Good Eating Habits:
- Eat small portions of food at a time. Avoid stooping or bending soon after eating. Eat and wait for 2 to 3 hours before lying down or sleeping
- Good Pill-taking habits:
- Always take your pills with enough water (at least a glass of water). Take your pills standing or sitting upright and wait for at least 30 minutes before lying down.
- Lose Extra Weight:
- If you are overweight or obese, the weight around your abdomen can push your stomach upwards. This increases your risk for reflux esophagitis and worsens your symptoms. Losing extra weight and maintaining a healthy weight help relieve symptoms and prevent recurring problems.
- Quit or Avoid Smoking:
- Tobacco contains nicotine that weakens the LES and increases the risk for GERD, reflux esophagitis, and eosinophilic esophagitis.
- Elevate Your Head:
- Raise the head of your bed by 6-8 inches or sleep with your head on specially designed wedge pillows. Using pillows isn’t effective against acid reflux.

- Avoid Certain Medications:
- Avoid some medications like pain-relievers, antibiotics, and other indicated drugs.
- Use Herbal Remedies:
- These should be used only after you have gotten a go-ahead from your doctor. Their dosage should also be discussed with your doctor. These may be used for reflux symptoms- licorice, ginger root, chamomile, peppermint oil, slippery elm, and marshmallow.
Untreated and Long Term Consequences
Left untreated, esophagitis can lead to changes in the structure of the esophagus. Possible complications include:
- Esophageal Stricture:
- This refers to the scarring or narrowing (stricture) of the esophagus. In this condition, prolonged deep injury results in fibrotic scarring and abnormal tissue growth (neoplasia). The esophagus becomes narrow, making it difficult to swallow.
- Barrett’s Esophagus:
- In this condition, the lining of the esophagus becomes thicker and reddened. The cells lining the esophagus change and become like the cells lining the intestine. It is a risk factor for esophageal cancer.
- Damage to the esophageal tissue from retching (if food gets lodged) or during endoscopy (due to inflammation).
Upcoming Treatments
- Eosinophilic Esophagitis:
- New biologic treatment options are being developed to treat eosinophilic esophagitis. They are expected to be available in a few years. These medications stimulate the body’s immune system to fight infection, inflammation, or disease.
Conclusion
Esophagitis is the inflammation that may damage tissues of the esophagus, resulting in chest pain and difficulty swallowing. It is caused by acid reflux, allergens, infections, and certain medications. Management of esophagitis depends on the cause and the severity of the condition.
Sources:
Healthline website. https://www.healthline.com/health/esophagitis
Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/esophagitis/symptoms-causes/syc-20361224