When you have open sores in any of your lower esophagus, the lining of your stomach, or small intestine, you have a peptic ulcer. Peptic ulcers are a relatively common health problem. The most common symptom is abdominal discomfort or pain.

Introduction
Peptic ulcers develop when the gastric acids erode the mucus lining (the protective layer) of your digestive tract. They may also be caused by inflammation caused by the bacteria, Helicobacter pylori (H. pylori).
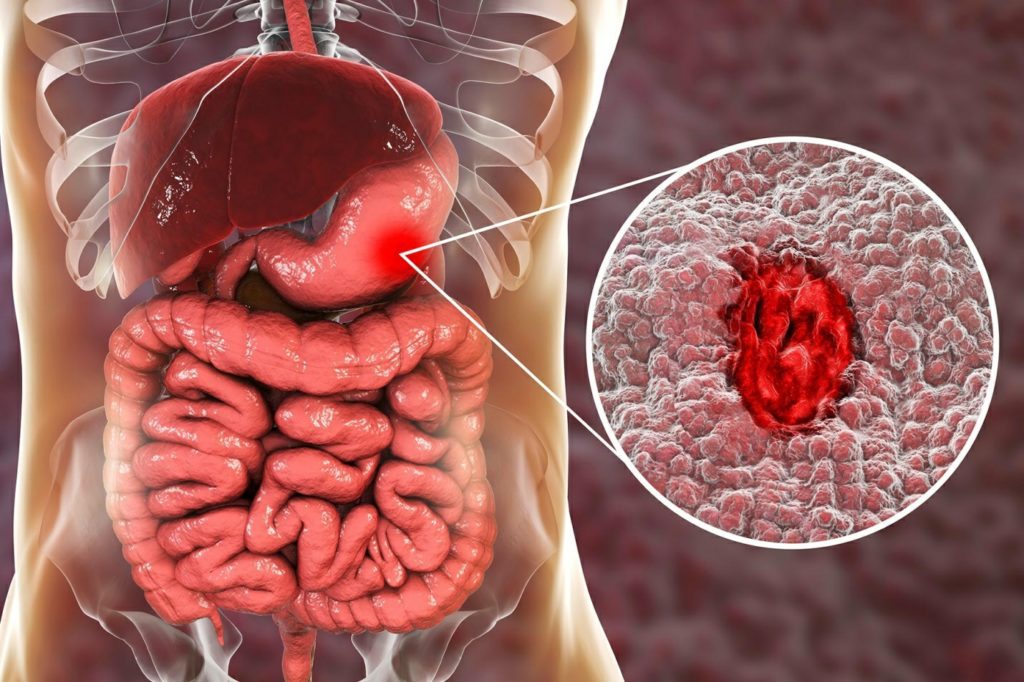
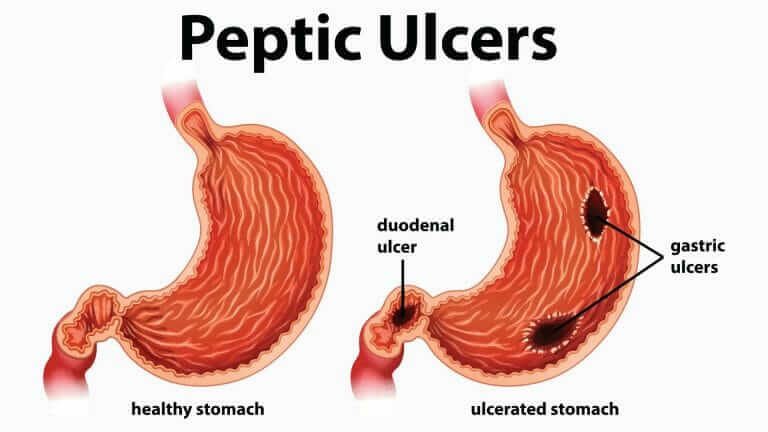
Peptic ulcers are open sores in your lower esophagus, the lining of your stomach, or the upper portion of the small intestine. Thus, there are three types of peptic ulcers:
- Esophageal ulcers:
- These are ulcers that occur in the lining of your lower esophagus. These sores develop when the acidic contents of the stomach backflow into the esophagus and erode its lining. It is often located at the lower esophageal sphincter (LES) – the junction between the esophagus and the stomach. They make swallowing difficult (dysphagia) and can have severe complications.
- Gastric ulcers:
- These are ulcers that occur within the (on the lining) stomach.
- Duodenal ulcers:
- These ulcers develop in the upper part of the small intestine- the duodenum. The small intestine is an organ concerned with digesting and absorbing food nutrients.
You may and may not have symptoms. The most common symptom is pain or a burning sensation in the abdomen. If left untreated or poorly managed, it may result in internal bleeding and other serious complications.
Causes of Peptic Ulcers
Ulcers form when the stomach acids etch away the lining of the esophagus, stomach, and small intestine.
The following are causes of peptic ulcers:
- Bacteria:
- This is the most common cause of peptic ulcers. It is called Helicobacter pylori (H. pylori). It is present in many people, however not all of those who have it develop ulcers. However, in some people, it increases the production of acid, wears away the protective lining, and irritates the digestive tract. H. pylori can be gotten via a human-to-human transmission (kissing), and contaminated food and water.
- Medications:
- Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) can predispose you to develop a peptic ulcer. This is due to these medications blocking the pathway for producing a chemical that protects the inner lining of your stomach and small intestine. Examples of NSAIDs include aspirin (Bayer), ibuprofen (Advil, Motrin IB, etc.), and naproxen sodium (Aleve). The risk for medication-induced peptic ulcer increases with female sex and advanced age above 60 years.
- Acid Reflux:
- The lower esophageal sphincter (LES) is the muscular junction between the esophagus and the stomach. It opens to allow food into the stomach after swallowing. Then, it closes to prevent the flow of gastric juices and food contents back into the esophagus. An ineffective LES allows the backflow of acidic stomach contents into the esophagus. Persistent acid reflux can erode the lining of the esophagus, cause inflammation and damage to the esophageal lining sores.
- Smoking:
- Smokers are at a higher risk of developing duodenal ulcers. Smoking cigarette interferes with the body’s natural protective mechanisms against stomach acid. This stomach acid is neutralized when it enters the duodenum of the small intestine by sodium bicarbonate. The pancreas produces this sodium bicarbonate. In the long run, smoking increases the production of stomach acid and decreases the production of bicarbonate.
In the stomach, smoking also reduces the production of prostaglandins in the mucous lining of the stomach. Thus, the stomach mucosa is susceptible to ulceration. They are also at risk of esophageal ulcers. Nicotine relaxes the LES, thus encouraging acid reflux. Smoking also increases the risk of esophageal and stomach cancers that also affect the respective linings of the organs affected.
- Excess alcohol:
- Consuming too much alcohol can cause your stomach to produce more acid. Also, research has confirmed a relationship between H. pylori infection and excessive drinking of alcohol.
- Radiation therapy:
- Sores or lesions can develop from high-voltage radiation therapy.
- Old age:
- While ulcers can occur at any age, the advanced age of over 60 years is a major risk factor for peptic ulcers. This may be related to the reduced effectiveness of the body’s natural protective mechanisms against stomach acids.
- Other medications:
- Taking drugs such as steroids, selective serotonin reuptake inhibitors (SSRIs), alendronate (Fosamax), anticoagulants, and risedronate with NSAIDs can increase your risk for peptic ulcers.
The following do not cause peptic ulcers but they can worsen your symptoms:
- Eating spicy foods
- Untreated stress
Symptoms of Peptic Ulcers
Most people are asymptomatic-do not show symptoms. However, the most common symptom is a burning sensation/pain in your stomach. It usually extends from the navel (belly button) to the chest and can range from mild to severe. It may come and go for many days or weeks, lasting for a few minutes or a few hours at a time.
The burning abdominal pain often worsens with increased production of stomach acid, having an empty stomach, after taking an NSAID medication, or after drinking citrus juice, alcohol, or coffee. Taking antacids or eating foods like yogurt, turmeric, blueberries, bananas, fruits, and vegetables may relieve symptoms. The pain may be worse at night or between meals.
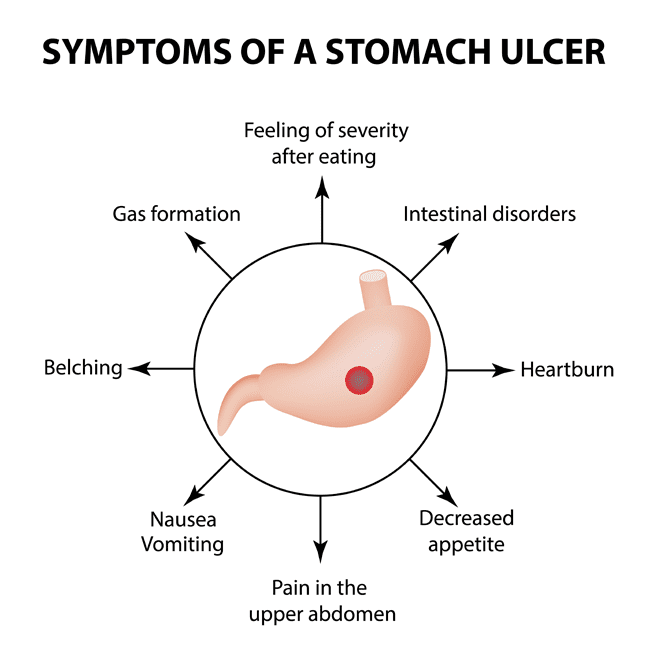
Other symptoms of peptic ulcers include:
- Full or bloated feeling
- Belching or burping
- Intolerance to fatty foods
- Heartburn
- Chest pain
- Nausea
- Vomiting or vomiting blood which may be red or black
Less common symptoms include:
- Dark-colored or blood-stained stools- may be black or tarry.
- Difficulty breathing
- Feeling faint
- Indigestion
- Unexplained weight loss
- Appetite changes
Medications for Peptic Ulcers
Treatment for peptic ulcers depends on the cause. The treatment usually is aimed at one or more of the following:
- killing the bacteria, H. pylori
- eliminating or reducing the use of NSAIDs
- helping your ulcer heal with medications by reducing stomach acid
- coating the protective lining of your stomach and small intestine

- Antibiotics:
- If your ulcer is because of an H. pylori infection, your doctor may prescribe antibiotics to kill the bacteria. Examples of antibiotics include clarithromycin (Biaxin), amoxicillin (Amoxil), metronidazole (Flagyl), tinidazole (Tindamax), tetracycline, and levofloxacin.
- Usually, proton pump inhibitors (PPIs) and sometimes bismuth subsalicylate (Pepto-Bismol) will be prescribed with these antibiotics. These medications help decrease stomach acid production. These regimens maybe triple or quadruple therapy. Triple therapy involves the combination of two antibiotics (amoxicillin and clarithromycin) with a PPI. If you are allergic to penicillin (such as amoxicillin), your doctor may replace it with metronidazole (Flagyl).
- A quadruple therapy treatment may be recommended if you’ve taken these drugs repeatedly or you live in an area with high antibiotic resistance rates. This includes two antibiotics, a PPI and bismuth subsalicylate. You are to take the regimen (any of them) for two weeks (10-14 days). You may suffer minor side effects from the antibiotics including diarrhea and stomach upset.
- Proton-pump inhibitors (PPIs):
- If your ulcer is due to overproduction of stomach acid, your doctor may prescribe proton-pump inhibitors (PPIs). These medications reduce stomach acid by blocking the pathway of acid production by stomach cells and encourage healing. Some are available as over-the-counter (OTC) while some are on prescription. Examples include lansoprazole (Prevacid), omeprazole (Prilosec), esomeprazole (Nexium), rabeprazole (Aciphex), and pantoprazole (Protonix).
- Long-term use of these medications at high doses may increase your risk of hip, wrist, and spine fracture. Talk to your doctor about whether a calcium supplement may help lower this risk.
- Histamine (H2) blockers:
- These medications are also called acid blockers. They relieve ulcer pain and help your ulcer heal by reducing the release of acid into your digestive tract. Examples are famotidine (Pepcid), cimetidine (Tagamet), nizatidine (Axid AR), and ranitidine. They are available as a prescription and also over the counter in lower doses.
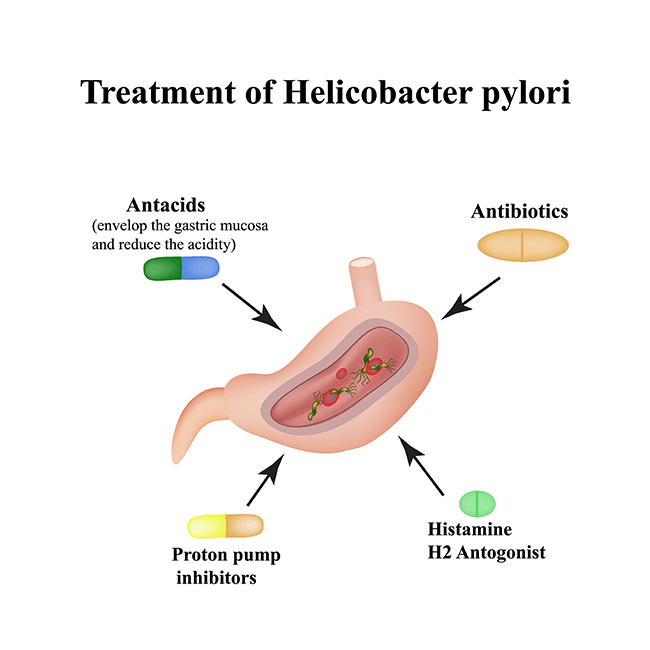
- Antacids:
- Your doctor may include an antacid in your drug regimen. This group of medications helps neutralize stomach acids with alkaline chemicals. Examples of aluminum hydroxide (ALternaGEL, Amphojel) and magnesium hydroxide (Phillips Milk of Magnesia, Phillips Chewable). Side effects can include constipation or diarrhea, and altered magnesium and calcium metabolism. Antacids do not heal your ulcer, they only provide rapid pain relief.
- Cytoprotective agents:
- These medications line your stomach and small intestine, thus protecting their cells and tissues from stomach acids. Examples are sucralfate (Carafate) and misoprostol (Cytotec). They coat your stomach and reduce symptoms of peptic ulcers.
Surgeries for Peptic Ulcers
Surgery may be required for ulcers that fail to heal with medical treatment (refractory ulcers) or it keeps recurring. Also, surgeries may be needed for complications like bleeding ulcers, perforation, and obstruction.
For bleeding ulcers or hemorrhaging ulcers, surgery will be used to identify the source of the bleeding and stop it. Usually, it is an artery present at the site of the ulcer. Perforations require emergency surgeries to close the holes in the walls of the organ-esophagus, stomach, and duodenum.
Surgery can also be done to lower the amount of stomach acid. This surgery however has severe complications that will be discussed with your doctor.
Approaches to these surgeries include:
- Open Laparotomy:
- Involves making a large abdominal incision to open up the abdomen.
- Minimally invasive laparoscopic surgery:
- Involves making a small abdominal incision and using a laparoscope- a camera-equipped surgical device that transmits images and is used for the repair.
- Endoscopy:
- Involves using a flexible tube that is inserted into the throat and passed down the esophagus and stomach to repair an ulcer. The tube has a camera and enables the use of surgical tools.
Types include:
- Graham Patch:
- This surgery can be done as an open laparotomy and laparoscopic surgery. In this surgery, the omentum- the fatty tissue that covers the stomach and the intestine is cut and used to close a small perforation.
- Partial Gastrectomy:
- This involves cutting a small portion of the stomach where the ulcer is located away. This procedure is carried out when the ulcer is big and deep. So the affected part is resected and other parts are stitched together. This surgery can be done via open laparotomy or laparoscopy.
- Vagotomy:
- In this surgery, one or more branches of the vagus nerve are cut away. This is done to reduce stomach acid.
Lifestyle Changes for Peptic Ulcers
The following lifestyle modifications can help prevent and/or relieve symptoms:
- Watch your diet and eating habits:
- It is best to do the following:
- Eat a balanced diet
- Eat smaller meals 6-7 times daily
- Eat slowly
- Sit upright while eating after meals
- Eat 2-3 hours before bedtime
- Avoid taking alcohol
- Avoid trigger foods such as alcohol, coffee, and caffeinated beverages, spicy foods, etc.
- Eat more food with probiotics such as yogurt, miso, cheese, and sauerkraut.
- Quit smoking:
- Smoking cigarettes or tobacco will slow your healing process and increase the risk for recurring ulcers.
- Avoid and manage stress:
- Stress is a risk factor for ulcers and can worsen symptoms. Thus, avoiding stress and managing existing stress is important.
- Avoid NSAIDs:
- Substitute NSAIDs with acetaminophen (Tylenol) for pain relief. Take all medications with plenty of water.
Untreated and Long Term Consequences of Peptic Ulcers
Left untreated, peptic ulcers can have serious consequences. Possible complications include:
- Internal bleeding:
- There can be internal bleeding. It can be slow and long-term leading to anemia. Significant blood loss may require hospitalization or a blood transfusion. Signs of bleeding ulcers include
- Dizziness
- Breathlessness
- Fatigue
- Lightheadedness
- Pallor (looking pale)
- Heart palpitations
- Fainting
- Black or bloody vomit
- Black, bloody, or tarry stools
- Perforation:
- Untreated ulcers can cause a hole in the wall of the esophagus, stomach, or small intestine. This can cause a more serious crisis as it allows bacteria to enter or the infection to spread to your peritoneum. The infection of the peritoneum (lining of your abdomen) is called peritonitis. Peritonitis is an infection that can quickly spread to the bloodstream and cause sepsis. Sepsis can cause multiple organ failure and death. Signs of peritonitis are acute, sharp abdominal pain that gradually worsens and hard, distended abdomen.
- Obstruction:
- In some cases, peptic ulcers can be swollen or scarred and block food as it passes through your digestive tract. This can bring about symptoms such as:
- Feeling full easily or bloated
- Frequent vomiting
- Weight loss
- Cancer:
- The bacterium, H. pylori in the stomach is a carcinogen and untreated infection can progress into stomach cancers. Duodenal ulcers rarely develop and become cancers.
The above complications are serious and may require surgery. Seek urgent medical attention or call 911 if you have an ulcer and notice any of the following:
- Symptoms of anemia such as dizziness, looking pale, weakness or fatigue. Your ulcer may have progressed to a bleeding ulcer.
- Sharp abdominal pain, severe back pain, or a firm, distended abdomen. You may have perforated the wall of your digestive tract and have peritonitis.
- Vomit that is bloody, like coffee-grounds or dark red. Your ulcer may be bleeding.
- Stool that is black, dark, or tarry and sticky. You may have internal bleeding.
- Feeling cold, clammy, or faint. You may have lost significant amounts of blood and be in shock.
Upcoming Treatments for Peptic Ulcers
There are currently no stated upcoming treatments for peptic ulcers.
Conclusion
Peptic ulcers are sores in the lining of any of the esophagus, stomach, or duodenum of the small intestine. It is commonly caused by H. pylori infection or long-term use of NSAIDs. Prevention is by protecting yourself against infections and using NSAIDs with caution. Peptic ulcers, although a fairly common digestive tract disorder, can have serious consequences.
Treatment is majorly medical. However, some ulcers fail to heal. These are sometimes a result of regular tobacco, regular use, and/or abuse of pain relievers especially NSAIDs and some H. pylori infections are resistant to antibiotics.
Sources:
https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/symptoms-causes/syc-20354223


