Inflammatory bowel disease is a disease that targets the bowel. It pursues a protracted, relapsing, and remitting course. According to the Crohn & Colitis Foundation of America (CCFA), Approximately 1.6 million Americans currently have IBD, a growth of about 200,000 since the last time CCFA reported this figure (in 2011).
As many as 70,000 new cases of IBD are diagnosed in the United States each year. Symptoms that accompany this condition include abdominal pain, diarrhea, fatigue, cramping, bloating, etc.
Introduction
Inflammatory Bowel Disease (IBD) has no exact definition and also defies cure. At best, it can be defined as a condition usually associated with an immune system dysregulation, i.e., when the immune system is overreacting. The immune system is responsible for fighting off harmful diseases and plays an important role in watching for infection. It turns itself up to fight and turns itself down when the infection is gone. However, in IBD, it is turned up when it shouldn’t be and thus fights off every microorganism, either harmful or harmful. The immune system behavior can lead to soreness and inflammation in the intestine and sometimes other areas like the eyes, liver, skin, or joints.
IBD is not your fault, and you didn’t do anything to make it happen. Some people feel alone and isolated when diagnosed with IBD, and it is important to talk to someone. It is important to know that you are not alone. There are over 1.6 million people in the US and over 2 million people in Europe with IBD.
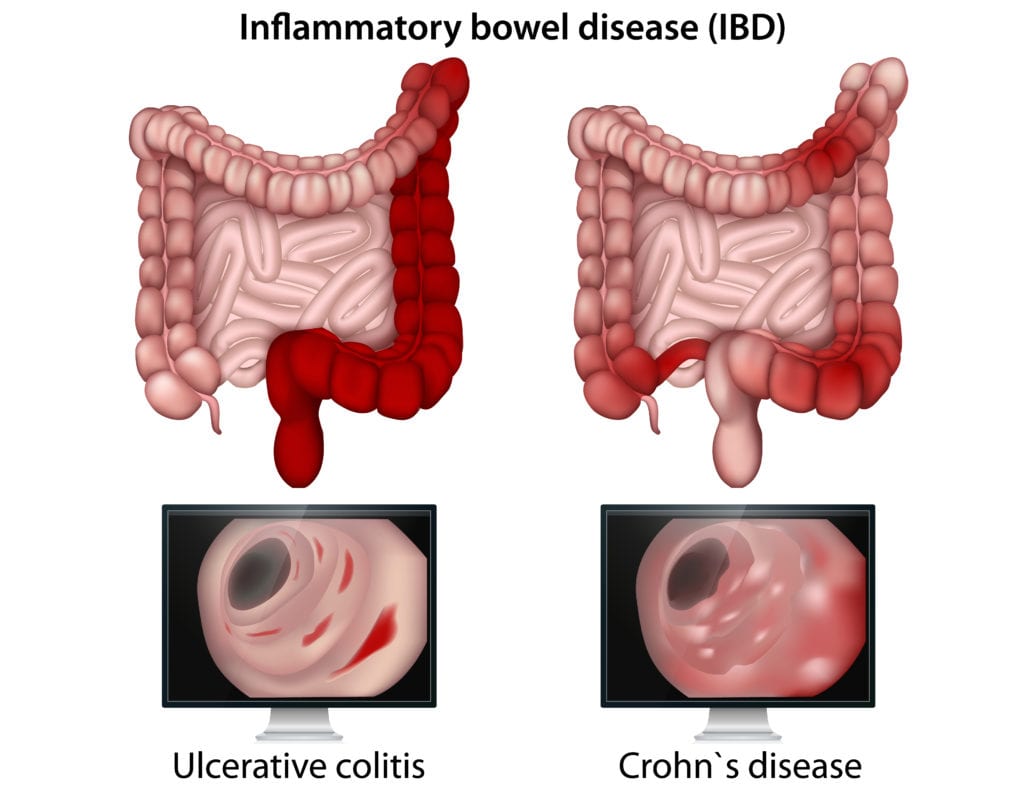
It is not a singular disease, but it instead refers to two related but distinct diseases. One is called Crohn disease (CD), and the other is Ulcerative colitis (UC). The key differences are in the location of the inflammation and also the extent of it. We will understand these individual diseases, their causes, symptoms, treatment, and pathology.
Ulcerative Colitis
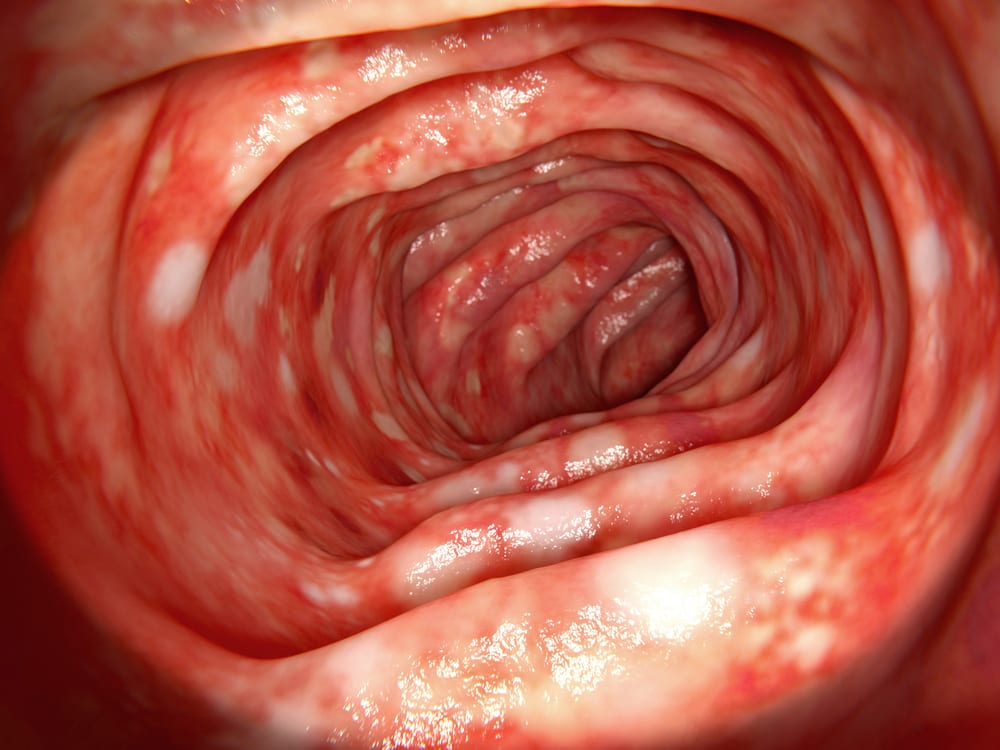
Colitis is the inflammation within the large intestine or the colon. Ulcerative colitis is a type of IBD that leads to ulcers forming along the lumen or inner surface of the rectum, colon, and large intestine.
These ulcers are points in the mucosa, anywhere the tissue has eroded and left behind breaks or open sores in the membrane. At times, there may be a flare that is the result of new damage that has happened. There are occasions when remission occurs, and the tissue starts to heal up.
Ulcerative colitis is the most common type of inflammatory bowel disease. The types are not many, but this causes inflammation and ulcers in the mucosa and submucosa of the large intestine only. This sets it apart from Crohn’s disease, another inflammatory bowel disease.
Causes Of Ulcerative Colitis
Although a few environmental conditions like stress and diet were once believed to be the etiologies behind the formation of these ulcers in the gut, now, it’s thought that these are more secondary – meaning that they seem to make symptoms worse. Still, ulcerative colitis is now ultimately considered to be autoimmune in origin.
T-Cells
The immune system’s cytotoxic T-cells are usually present in the epithelium lining along the colon. A school of thought is that ulceration and inflammation in the large intestine result from T-cells damaging the cells lining along the large intestine’s walls, resulting in these eroded points or ulcers.
It’s not apparent what exactly these T-cells are expected to be targeting, though. Some patients test positive for p-ANCAs (perinuclear antineutrophil cytoplasmic antibodies) in their blood. These are a kind of antibodies that target antigens in the body’s neutrophils.
Gut Bacteria
Another school of thought theorizes that this may be partly due to immune reaction to some gut bacteria, which has some structural similarity to our cells, allowing antibodies to those gut bacteria, or p-ANCAs, to “cross-react” with neutrophils.
Some patients, however, seem to carry a larger amount of gut bacteria that secretes sulfides. And in most cases, high sulfide production is connected with periods of active inflammation instead of periods of remission.
Ultimately, though, these are mostly correlations in theories, and we’ve yet to nail down the specific mechanism behind mucosal destruction.
Combination
The cause is ultimately some combination of environmental stimuli, perhaps the sulfide-producing bacteria, mixed with a genetic predisposition. Patients with a family medical history of ulcerative colitis are more prone to developing the disease themselves.
With ulcerative colitis, the pattern for ulcerations seems to be precise and continuous. It means that the inflammation goes around the whole lumen, starts in the rectum, and continues along the large intestine. This is without any apparent breaks or any unaffected tissue. It is like it’s working its way from one end to the other.
Symptoms for ULCERATIVE COLITIS
Pain
As more damage is done to the tissue, patients experience pain in the left lower quadrant, corresponding to the rectum.
Diarrhea and blood in the stool
This is a more severe and frequent bout of diarrhea. Sometimes with blood in the stool. As mucosa and epithelium are destroyed, patients might release blood in serum into the lumen, contributing to the blood witnessed in the stools. Additionally, one of the chief jobs of the large intestine is the absorption of water, so as these cells are damaged, the large intestine will not be able to perform this role efficiently, thereby letting too much water through. This contributes to diarrhea.
Other Symptoms Include:
- Weight loss
- Decreased Appetite
- Night sweats
- Fever
- Tiredness
- Nausea/ Vomiting
- Fecal urgency
- Fecal incontinence
- Tenesmus (the inability to empty the bowels, despite the urge)
Occasionally, it can affect or inflame other parts of your body, such as your eyes, skin, liver, and joints. Other symptoms can be more specific. For example, because UC only affects the inner lining of the bowel, we tend to see mucus and blood in the stool. Whereas Crohn can inflame the whole bowel wall, there may be blood, and significant abdominal pain, nausea, and vomiting. Both diseases can lead to growth delays in children.
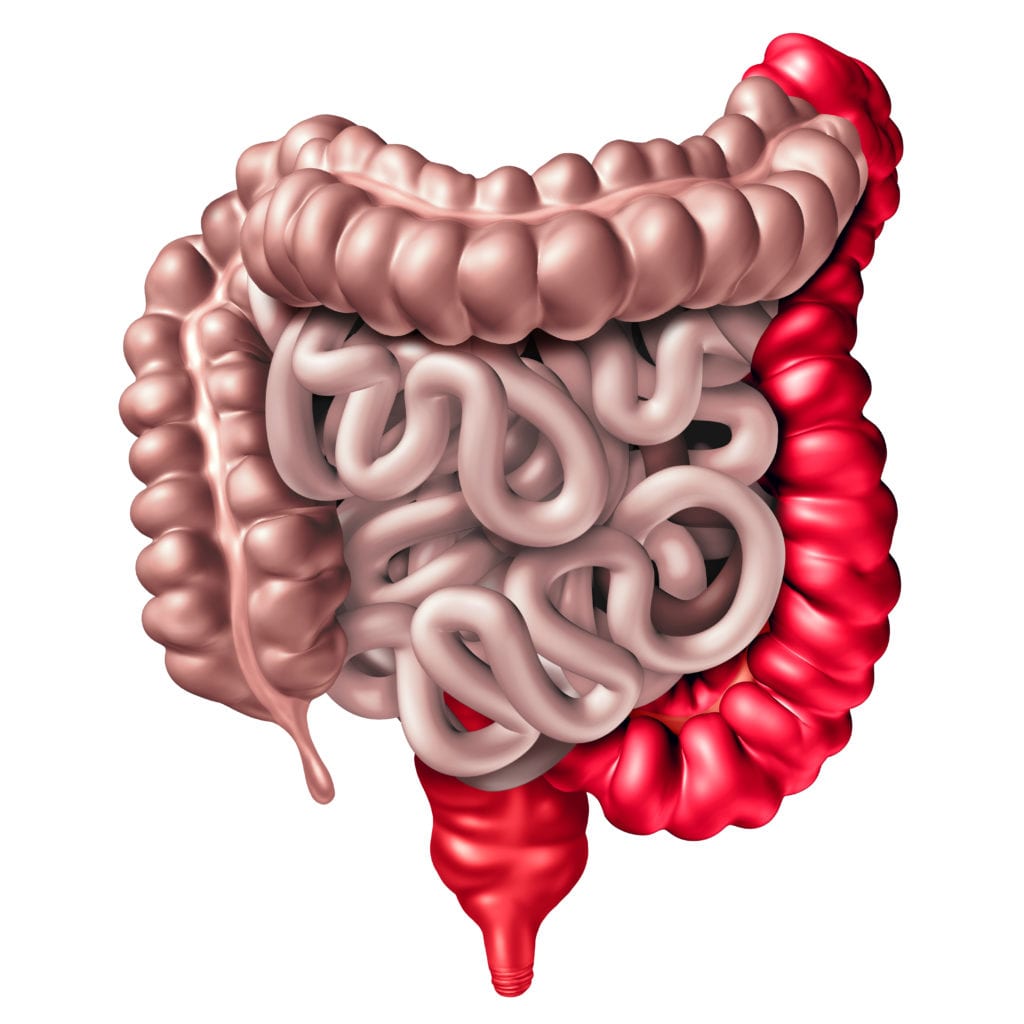
Ulcerative colitis is also sub-divided based on the areas it affects in the colon.
- Proctitis: This affects the rectum only.
- Proctosigmoiditis: This affects the rectum only and the sigmoid colon.
- Left-sided colitis: This affects the rectum, sigmoid colon, and descending colon.
- Pancolitis: This affects the entire colon.
It is mildest in Proctosis and most severe in Pancolitis.
Ulcerative Colitis Diagnosis
Colonoscopy
Diagnosis of ulcerative colitis typically requires colonoscopy, which is when a long tube with a camera at the end is inserted retrograde through the anus and into the rectum and colon to see the ulcers and take a biopsy.
Radiological Imaging
This involves using more technologically advanced methods like the CT scan, MRI. A barium enema (which is where a liquid is injected into the rectum through a small tube) and an X-ray are taken to look for abnormalities in the large intestines.
SURGERIES AND MEDICATIONS FOR ULCERATIVE COLITIS
The treatment adopted depends on the severity of the symptoms. Although there is no cure, Doctors can properly manage it; treatments include:
Medications
Anti-Inflammatory medications like sulfasalazine or mesalamine are given. Doctors might prescribe drugs that suppress the immune system in difficult situations. These drugs are usually immunosuppressors like corticosteroids, azathioprine, or cyclosporine.
Biologics
If the medications fail, biological treatments can be adopted for those with moderate to severe inflammatory bowel disease. They function by utilizing specially developed antibodies to block selective effects of the molecules that participate in the inflammation of the gut wall. The idea here is that we can move beyond just symptom management and help treat the mucosal lining and healing it, thereby leading to remission and preventing relapses. Treatments like infliximab (which is a TNF inhibitor), adalimumab, and golimumab can be used.
Colectomy
Finally, if these treatment options fail, sometimes patients will have to undergo surgery. This surgery is called a “colectomy,” and it is the surgical excision of the colon. Because the disease only attacks the large intestine, removal of the colon generally remedies the condition. It would be advisable to weigh the advantages of curing the disease against the complete loss of the large intestine.
CROHN’S DISEASE
Crohn’s disease signifies a variation of IBD; in 1932, Crohn et al. published a paper that established CD as a distinct disease from UC.
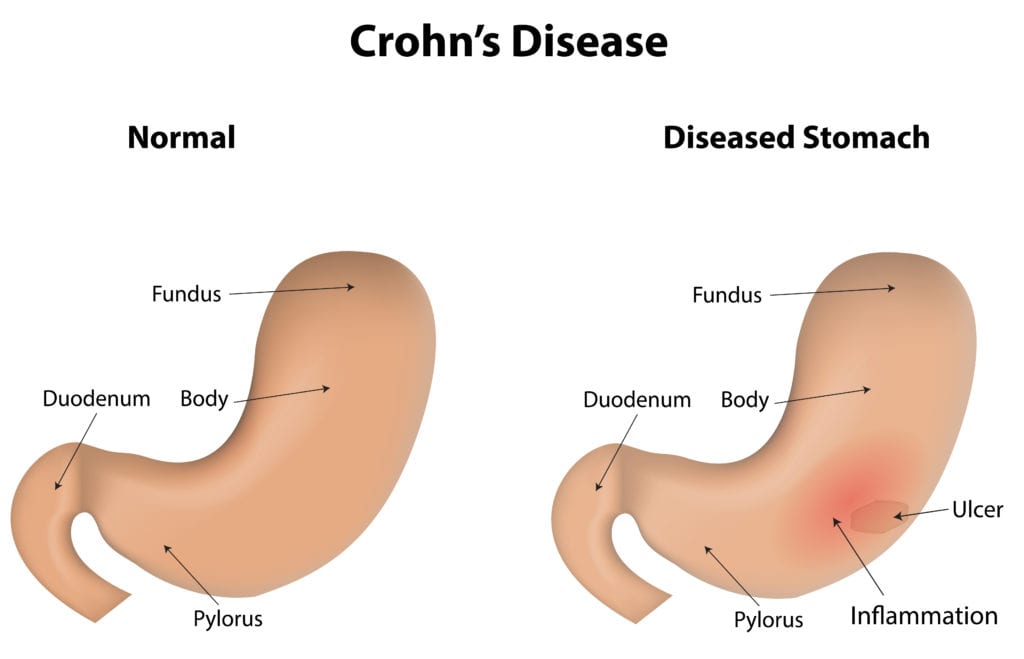
Chron’s disease is now classified as a disease characterized by inflammation that can affect any portion of the Gastrointestinal tract. That is any part from the mouth down to the anus.
Inflammation can extend right through the entire thickness of the bowel wall to the outermost layer of the digestive tract.
Crohn’s disease isn’t technically classified as an autoimmune disease but rather an immune-related disorder; this means that the immune system is assumed to be triggered by some foreign pathogen in the gastrointestinal tract. Pathogens such as:
- Mycobacterium Paratuberculosis
- Pseudomonas
- Listeria
The immune system is expected to react to foreign pathogens. We all agree that is its function, right? Well, yes and no. We can say yes because it targets any foreign assailants. We can also say no because the inflammatory response can be uncontrolled and large, leading to the damage of cells in the GI tract.
So what’s thought to happen is that one of these pathogens actuates the immune system by presenting an antigen. The message gotten by one of the gastrointestinal cells will be like, “here,” I guess this is an infectious molecule, and that’s okay because it is.
At that instant, TH1 cells, also known as T helper cells, swoop in and deliver cytokines – which are cell signaling molecules like:
- Tumor necrosis factor-alpha
- Interferon-gamma
This further animates the inflammatory response.
The presence of cytokines pulls inflammatory cells like macrophages, which begin delivering even more inflammatory substances like platelet-actuating factors, free radicals, and proteases, which effectively contribute to inflammation.
Although not definitively understood, it’s thought that one of the steps in this proceeding is dysfunctional and results in an out-of-control and chaotic inflammatory response for patients with Crohn’s disease.
Unregulated inflammation involves platelet-actuating factors, free radicals, and loads of proteases swimming about the gastrointestinal tissue, eventually prompting the damage of healthy tissue cells.
This dysfunctional immune response is believed to be a result of genetics, and in fact, patients with family members having Crohn’s disease are more susceptible to developing it themselves.
Gene mutation is also a contributing factor. A number of genes have been investigated and are believed to contribute to evolving of the disease.
For gene expression, it is usual for nucleotides to be read in groups of three. The addition of 1 or 2 nucleotides leads to shifting all the remaining nucleotides, which usually ends up in totally different amino acids being coded and probably a dysfunctional protein.
The damage and inflammation in Crohn’s disease extend beyond the submucosal layer and through the entire depth of the intestinal wall. Sometimes we refer to this as being transmural from mucosa to serosa.
Symptoms Of Crohn’s Disease
Pains
As more gastrointestinal tissue is damaged, patients might experience pain in the affected areas, most commonly in the right lower quadrant, which is associated with the ileum.
Blood In The Stool & Diarrhea
These are common symptoms that have their etiology as damaged intestinal wall tissue. These cells lose their capacity to re-absorb water if the large intestine’s walls are damaged. This leads to more water is being excreted, resulting in diarrhea.
Malabsorption
If the small intestine is the one that is taking the brunt of the damage, patients may have malabsorption issues. This is because the small intestines are super important for absorbing nutrients.
Other symptooms include:
- Weight loss
- Fatigue
- Loss of appetite
- Fever
- Nausea/Vomiting
Surgeries And Medications For Crohn’s Disease
Medications
Treatment for Crohn’s disease usually comprises antibiotics and anti-inflammatory drugs. Antibiotics are meant to help curb symptoms by diminishing bacteria levels present in your intestine, sometimes referred to as bacterial overgrowth. They also do so by controlling the immune response since some antibiotics have anti-inflammatory effects as well.
If patients have severe symptoms, they may be given immunosuppressants like corticosteroids.
Surgery
Removal of the affected tissue is possible, but one really important distinction from all sorts of colitis is that removal doesn’t cure the disease since the inflammation can occur anywhere along the GI tract.
Lifestyle Changes For IBD
Dietary Management
Avoid raw fruits and vegetables (cook them); non-dairy diets may help some people. Some people benefit from Nutrition Therapy (a special diet given via feeding tube or directly injected into the vein (intravenously)). The therapy provides nutrition while allowing the bowel to rest, reducing inflammation. Things to think about with the diet are pretty common sense and individualized. There is considerable variation from person to person, so self-awareness about what fruits set you off or work for you.
Staying Active
Staying active all the time is great. Not only does it get your mind off the disease and the impact it has on you, but you also get something out of it, whether it is taking a walk down the street or climbing.
Exercise
This is very important as it helps reduce stress. Other stress reduction methods can be very helpful, as is staying hydrated. Self-awareness is also important when it comes to managing stress. The unpredictability of IBD or dealing with symptoms, and at the same time dealing with life’s other stressors, can be incredibly tricky to navigate.
Untreated And Long-Term Consequences
If left untreated, complications to watch out for include:
- Increased risk for colon cancers
- Toxic colitis (fulminant colitis, toxic megacolon): This is a life-threatening condition characterized by sudden violent diarrhea, High fever, abdominal pains, and signs of peritonitis. It occurs when the inflammation extends into the smooth muscle layer of the intestinal wall, paralyzing the colon muscle.
Upcoming Treatments & Medications
Anti-Adhesion Molecules
Inflammation is facilitated by the migration of pro-inflammatory T cells into the gut, which is characteristic of CD and UC. Interaction between α4β1 and α4β7 integrins on lymphocytes and adhesion molecules allow for activated effector T cells to target the gut. T cells can travel out of the bloodstream and into the gastrointestinal tract as a result of this interaction.
Natalizumab (NAT) is a humanized IgG4 monoclonal antibody that prevents lymphocyte trafficking to the stomach and brain. It targets the α4-integrin subunit of α4β1 and α4β7 on the surface of lymphocytes.
Vedolizumab (VDZ) is a humanized IgG1 monoclonal antibody that inhibits leukocyte migration to the gut by specifically targeting the α4β7 integrin. It is approved for UC and CD.
Conclusion
Inflammatory bowel disease can have a strong effect on a person’s life physically, psychologically, and emotionally.
If you would like to try out some natural supplements to reset your stomach, we recommend Natural Colon. You will get immediate relief and potentially long-term relief.
Either at school or home and even in the place of work and having to go to the washroom more than ten times a day can be daunting; even talking about your bowels can be embarrassing. It can be challenging at any age but perhaps especially as a young person when this disease commonly strikes.
It’s a disease that often impacts families, not just individuals, and it is a journey that requires no small amount of bravery, problem-solving, and optimism. Although there is no cure yet, there are many treatment options available.
Lastly, it is important to remember that things will return to normal, even with the ups and downs.
Sources
Aufses AH Jr. The history of Crohn’s disease. Surg Clin North Am. 2001 Feb;81(1):1-11, vii. DOI: 10.1016/s0039-6109(05)70270-x. PMID: 11218157. https://www.sciencedirect.com/science/article/abs/pii/S003961090570270X?via%3Dihub
Crohn’s and Colitis Foundation Website. Environmental Triggers. https://www.crohnscolitisfoundation.org/research/challenges-ibd/environmental-triggers


